7 Scary Drug-Resistant Infections
1 / 8 Beware of Superbugs
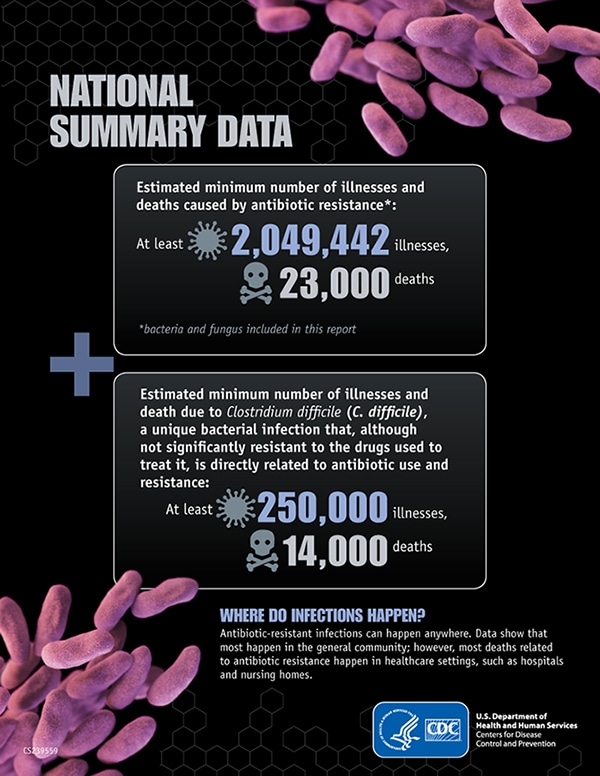
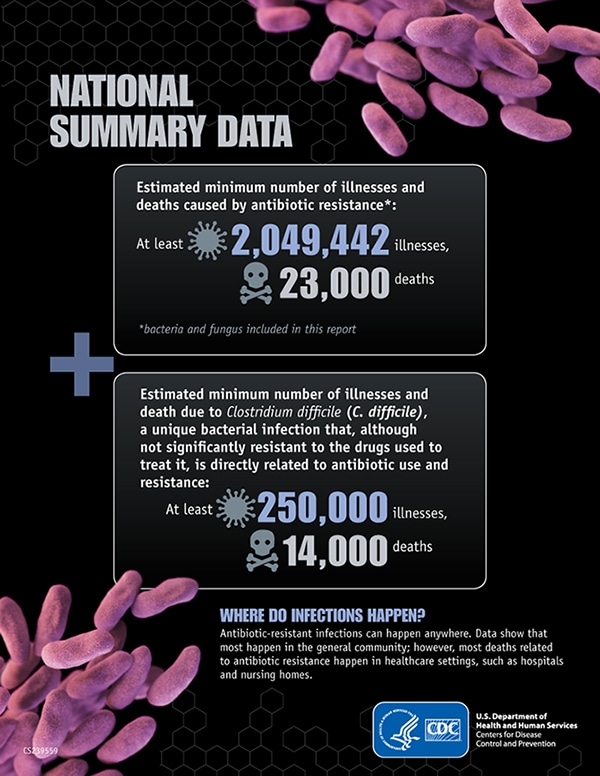
Antibiotic resistance is a growing public health concern. According to the Centers for Disease Control and Prevention (CDC), drug-resistant infections account for 2 million infections and lead to 23,000 deaths in the United States per year.Bacteria are experts at adapting to the drugs used to kill them, so when a course of antibiotics fails or isn’t completed, these bugs can come back with a vengeance. Fortunately, these infections can be avoided. Here are seven of the scariest drug-resistant infections, and how you can avoid them.
2 / 8 Clostridium Difficile (C. diff)
C. diff causes over 450,000 gut infections in the US each year, according to a study published in the New England Journal of Medicine. This bug can take over the gut when normal bacteria residents are booted out by antibiotics. The infection can cause painful cramping, inflammation, and diarrhea.The best way to avoid getting a life-threatening C.diff infection is to take antibiotics properly. There is also evidence that probiotic supplements could help prevent C. diff infection while taking antibiotics. C. diff can also be transferred by sharing a bathroom with someone who has it, so always practice good hygiene, especially when in healthcare settings. The CDC recommends contacting your doctor if you develop diarrhea within three months of taking antibiotics.
3 / 8 Carbapenem-Resistant Enterobacteriaceae (CRE)
CRE has been making headlines lately because of several recent deaths tied to CRE infection in hospitals in California and North Carolina. These bugs can infect the lungs, skin, bladder, and bloodstream, and are resistant to a class of antibiotics often used as a “last resort” against resistant bacteria in the enterobacteriaceae family. E. coli and Klebsiella are two more commonly known types of enterobacteriaceae.The CDC also ranks extended-spectrum beta-lactamase-producing enterobacteriaceae as a serious threat because they can resist common antibiotic drugs similar to penicillin. Since CRE is most often acquired in healthcare settings, preventing it depends on proper sanitation of medical devices and diligent hygiene among staff and patients. Don’t be afraid to ask your doctors and nurses if they’ve washed their hands before examining you.
4 / 8 Drug-Resistant Neisseria Gonorrhoeae
Neisseria gonorrhoeae are a group of sexually transmitted bacteria that cause urinary and reproductive tract infections, rectal infections, and can lead to infertility in men and women if left untreated. According to the CDC, the drugs available for treating these infections are dwindling. Fortunately, you can avoid drug-resistant gonorrhoeae by maintaining safe sex practices, like the proper use of condoms.5 / 8 Methicillin-Resistant Staphylococcus Aureus (MRSA)
Up to two percent of people carry MRSA in their noses or on their skin. However, if it spreads into an open wound, or the immune system can’t control it, then MRSA can cause severe skin infections and deadly bloodstream infections.Like CRE, MRSA can also be transferred through medical devices, but hospital-acquired cases have been dropping in recent years. To avoid MRSA, don’t share razors or other personal items, keep wounds clean and covered, and practice good hygiene – especially in settings where many people are sharing common spaces like summer camps, college dorms, or military barracks.
6 / 8 Streptococcus Pneumoniae
S. pneumoniae, which are most commonly spread through coughing, can cause ear and sinus infections, pneumonia, and meningitis. You can defend yourself against these infections by getting the pnuemococcal conjugate vaccine, which has already helped reduce the spread of drug-resistant S. pneumoniae. A more powerful form of the vaccine is recommended for adults over 65 – the age group with the highest risk of getting this infection.7 / 8 Drug-Resistant Malaria
Malaria is caused by a parasite that is transferred to humans through mosquito bites. There are five different parasites that can cause malaria. Three of those parasites have now developed resistance to antimalarial drugs. Malaria causes fever, fatigue, nausea, and vomiting. Malaria is the most deadly to children under the age of five. Though cases and deaths have dropped significantly in the last decade, the disease still caused approximately 584,000 deaths worldwide in 2013. The best way to avoid malaria is to sleep under a mosquito net when visiting a malaria-endemic area.8 / 8 Multi-drug resistant (MDR) and extensively drug resistant (XDR) Tuberculosis
Tuberculosis is the second biggest infectious cause of death worldwide, according the World Health Organization. The CDC estimates over 1,000 drug-resistant tuberculosis cases occurred in the US in 2013. Worldwide, MDR cases have reached over 480,000 and only about half of patients with MDR tuberculosis can be cured. Tuberculosis, which is spread by coughing and sneezing, is most dangerous for people with weakened immune systems in settings where many people are crowded together, like nursing homes, homeless shelters, and prisons. Because tuberculosis can be carried without any symptoms for years, those at risk can be tested to determine if they’ve been exposed.
Antibiotics and similar drugs, together called antimicrobial agents,
have been used for the last 70 years to treat patients who have
infectious diseases. Since the 1940s, these drugs have greatly reduced
illness and death from infectious diseases. However, these drugs have
been used so widely and for so long that the infectious organisms the
antibiotics are designed to kill have adapted to them, making the drugs
less effective.
Each year in the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics and at least 23,000 people die each year as a direct result of these infections.
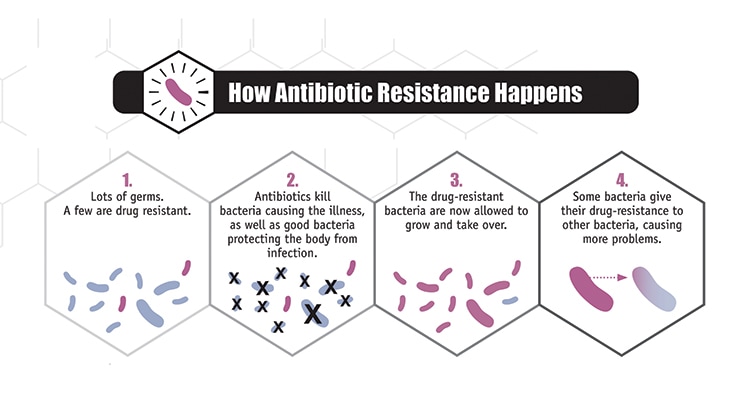
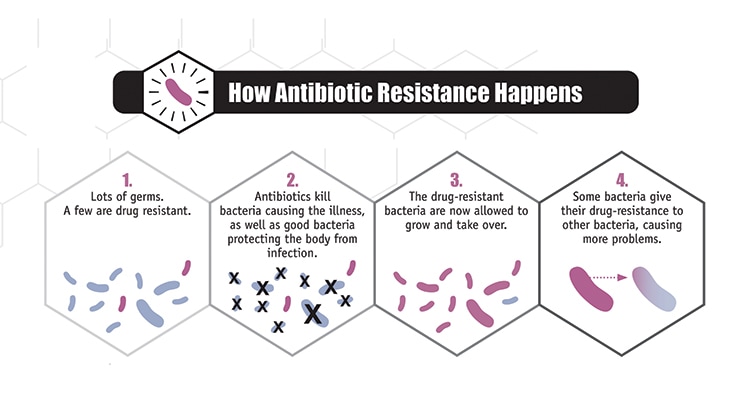
Antibiotic / Antimicrobial resistance is the ability of microbes to resist the effects of drugs – that is, the germs are not killed, and their growth is not stopped. Although some people are at greater risk than others, no one can completely avoid the risk of antibiotic-resistant infections. Infections with resistant organisms are difficult to treat, requiring costly and sometimes toxic alternatives.
Bacteria will inevitably find ways of resisting the antibiotics developed by humans, which is why aggressive action is needed now to keep new resistance from developing and to prevent the resistance that already exists from spreading.


Click here to enlarge image[PDF - 1 page]
Click here to enlarge image[PDF - 1 page]
Top of Page




Click here to enlarge image[PDF - 1 page]
Top of Page
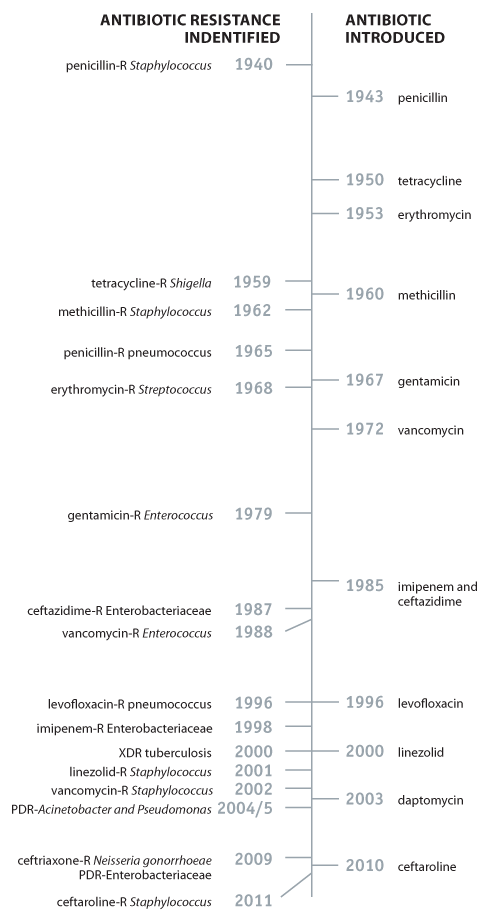
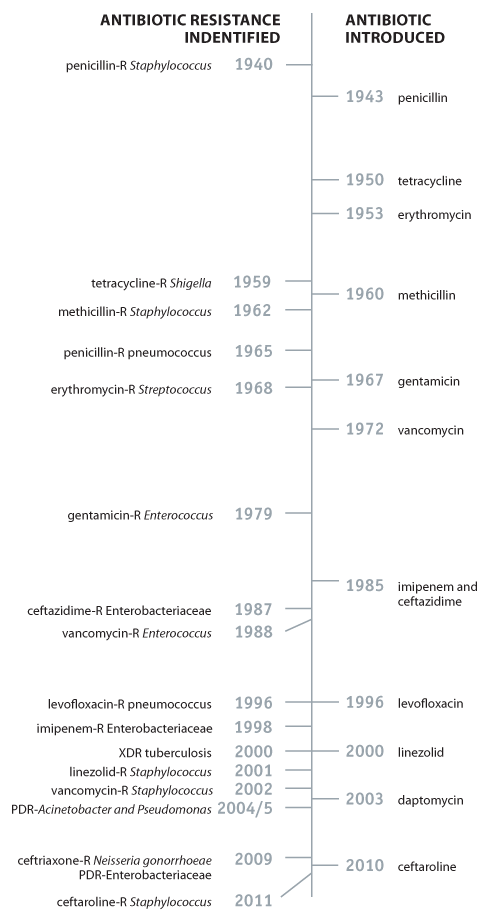
Penicillin, the first commercialized antibiotic, was discovered in 1928 by Alexander Fleming. While it wasn’t distributed among the general public until 1945, it was widely used in World War II for surgical and wound infections among the Allied Forces. It was hailed as a “miracle drug” and a future free of infectious diseases was considered. When Fleming won the Nobel Prize for his discovery, he warned of bacteria becoming resistant to penicillin in his acceptance speech.
Click here to enlarge image[PDF - 1 page]
Top of Page
Each year in the United States, at least 2 million people become infected with bacteria that are resistant to antibiotics and at least 23,000 people die each year as a direct result of these infections.
Antibiotic / Antimicrobial resistance is the ability of microbes to resist the effects of drugs – that is, the germs are not killed, and their growth is not stopped. Although some people are at greater risk than others, no one can completely avoid the risk of antibiotic-resistant infections. Infections with resistant organisms are difficult to treat, requiring costly and sometimes toxic alternatives.
Bacteria will inevitably find ways of resisting the antibiotics developed by humans, which is why aggressive action is needed now to keep new resistance from developing and to prevent the resistance that already exists from spreading.
Explanation of Bacteria and Other Microbes
Microbes are organisms too small for the eye to see and are found everywhere on Earth. There are many types of microbes: bacteria, viruses, fungi, and parasites. While most microbes are harmless and even beneficial to living organisms, some can cause disease among humans, other animals, and plants. These disease-causing microbes are called pathogens; sometimes they are referred to as “germs” or “bugs.” All types of microbes have the ability to develop resistance to the drugs created to destroy them, becoming drug-resistant organisms.
How Resistance Happens and Spreads
The use of antibiotics is the single most important factor leading to antibiotic resistance around the world. Simply using antibiotics creates resistance. These drugs should only be used to manage infections.Trends in Drug Resistance
- Antibiotics are among the most commonly prescribed drugs used in human medicine and can be lifesaving drugs. However, up to 50% of the time antibiotics are not optimally prescribed, often done so when not needed, incorrect dosing or duration.
- The germs that contaminate food can become resistant because of the use of antibiotics in people and in food animals. For some germs, like the bacteria Salmonella and Campylobacter, it is primarily the use of antibiotics in food animals that increases resistance. Because of the link the between antibiotic use in food-producing animals and the occurrence of antibiotic-resistant infections in humans, antibiotics that are medically important to treating infections in humans should be used in food-producing animals only under veterinary oversight and only to manage and treat infectious disease, not to promote growth.
- The other major factor in the growth of antibiotic resistance is spread of the resistant strains of bacteria from person to person, or from the non-human sources in the environment.

Click here to enlarge image[PDF - 1 page]
Resistance in the United States
Click here to enlarge image[PDF - 1 page]
Top of Page
Four Core Actions to Fight Resistance




Click here to enlarge image[PDF - 1 page]
Top of Page
Brief History of Antibiotics
Humans developed antimicrobials to destroy disease-causing microbes. The most commonly known antimicrobials are antibiotics, which target bacteria. Other forms of antimicrobials are antivirals, antifungals, and antiparasitics.Penicillin, the first commercialized antibiotic, was discovered in 1928 by Alexander Fleming. While it wasn’t distributed among the general public until 1945, it was widely used in World War II for surgical and wound infections among the Allied Forces. It was hailed as a “miracle drug” and a future free of infectious diseases was considered. When Fleming won the Nobel Prize for his discovery, he warned of bacteria becoming resistant to penicillin in his acceptance speech.
Click here to enlarge image[PDF - 1 page]
Top of Page
No comments:
Post a Comment